Osteoarthritis of the knee joint (otherwise known as gonarthrosis) is a fairly common disease, recently discovered not only in the elderly, but also in young people.
Pathology is one of the main reasons why patients who refuse to seek help from a traumatologist or orthopedist become disabled.
Let's look at why patients develop gonarthrosis of the knee joint, what are its main symptoms, how dangerous it is and how effective treatment is given for progressive destruction of the knee.
The main factors in the appearance of this pathology
Joints are constantly subjected to significant stress. The knees are particularly affected: they are forced to do significant physical work, so they wear out quickly. The process of deformation is intensified by the fact that the legs are forced to carry the weight of the body.
This fact contributes to the aging of the knees and the thinning and deterioration of the cartilage tissue of the joint.
The following reasons can accelerate the pathological process in the joints:
- Patients gain weight. Complete destruction of the joint occurs much faster and more intensively. It has been proven that obese people are three times more likely to have the disease than people of normal weight.
- Strong sports, so the joints are constantly damaged.
- Frequent fractures and previous knee injuries help the patient begin to degenerate articular cartilage processes at a fairly young age.
- Abnormalities in the bone area - the so-called valgus or varus deformity.
- Poor development of the ligamentous apparatus of the knee often leads to injuries and dislocations. The patient develops osteoarthritis due to the described injuries.
- Damage to the meniscus triggers the degenerative process of knee destruction.
- Constant stress leads to deterioration of the health of the musculoskeletal system.
- Disorders of metabolic processes in the body due to lack of food and minerals (bones suffer the most from calcium deficiency).
In addition, the following people belong to the risk group:
- all athletes;
- patients over 50 years of age, regardless of gender;
- menopausal women;
- patients suffering from varicose veins;
- persons with unfavorable inheritance.
What are the degrees of the disease?
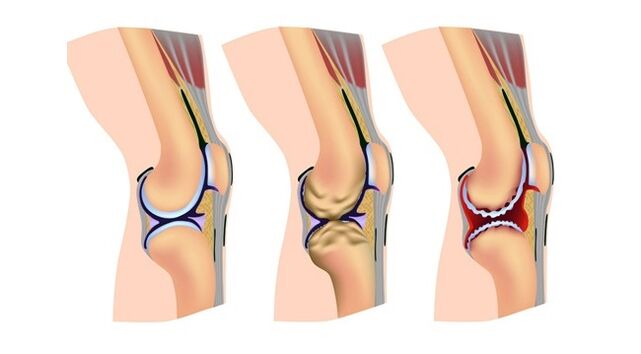
The pathology develops gradually, very slowly. It may not be visible at first, and the patient is in no hurry to see a doctor. However, the pathological process has already begun, and if not stopped in time, the functions of the lower extremities will gradually be lost, leading to the onset of disability.
Thus, in grade 1, the patient may notice that the foot is tired, even though the load is small. There are some limitations in the mobility of the knee joint, and a significant crisis is heard during movement.
Anxiety mainly has acute onset pains when not resting in the morning. After the patient "collapses", the anxiety gradually decreases, and increases again after sports activities. At this stage of the disease, no obvious deformation of bone tissue is observed.
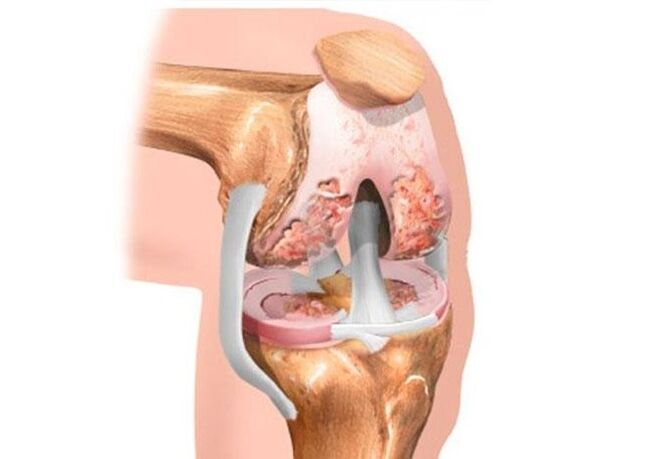
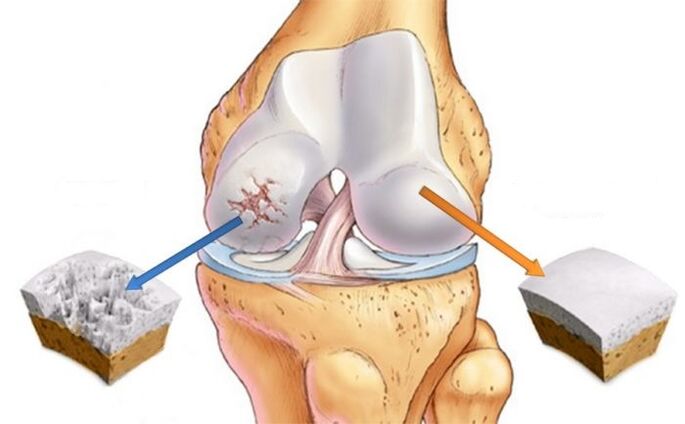
Grade 2 pain is exacerbated. That's why my place is broken. Sometimes it is almost impossible for the patient to move normally, and even after a light load, a long rest is required. As the joint space narrows, osteophytes grow in the bones, and pathological fluid accumulates in the joint.
In the 3rd grade, pain occurs not only during work and sports, but also in a state of complete rest. The deformation of the knee is very obvious, which complicates any movement.
General symptoms of the disease
It is necessary to pay attention to the general symptoms of osteoarthritis of the knee joint:
- Pain. It doesn't appear suddenly, but the slight discomfort can last for years. More severe pain is caused by trauma.
- Deformation of the knee (retains its previous shape).
- Accumulation of fluid in the intraarticular space. When its amount exceeds certain values, Baker develops a cyst. A tight elastic object appears behind the knee. It is most noticeable when the joint is extended.
- If the pathology is in the second or third stage, knee collapse is observed. It is significantly different from what is observed in a healthy person when the knee is bent or stretched. It feels as hard and painful as sound. Sometimes crunchy movements interfere with active movements.
- Decreased normal range of motion in the joint. Usually the patient cannot bend or open the affected leg. He is able to bend it at a right angle, and subsequent movements are accompanied by severe pain.
- Knee stiffness occurs primarily in stage 3. Sometimes patients can only walk with bent limbs.
- Increased pain when the weather changes.
- Significant thinning of cartilage. Occasionally, in advanced cases, bone exposure is noted. X-ray of the knee shows a significant accumulation of osteophytes.
Types of osteoarthritis
Depending on its origin, osteoarthritis is primary (continues as an independent disease) or secondary - a complication of existing pathologies. Depending on the location, the pathology is right, left and bilateral.
The following types of disease differ depending on the characteristics of the manifestation.
- A chronic course of deforming osteoarthritis is characterized by irreversible changes in the joint.
- Patellofemoral osteoarthritis develops as a result of long-term intense physical exertion.
- Inflammatory osteoarthritis occurs as a result of an inflammatory process in the joints that has not been treated for a long time.
- Dysplastic osteoarthritis develops due to congenital anomalies in the structure of the knee joint.
- Post-traumatic osteoarthritis occurs as a result of frequent damage to the musculoskeletal system.
- Metabolic osteoarthritis occurs with gout and other metabolic diseases.
- Postinfectious osteoarthritis occurs as a result of inflammatory pathologies that are not adequately treated.
- The static form of the disease is detected when the knees are under constant increasing pressure.
- When the cause of a knee lesion is unknown, experts talk about idiopathic osteoarthritis.
Features of the treatment of the disease

In the early stages of the disease, a rheumatologist and traumatologist are involved in treatment. If he has advanced too far, the patient should consult a surgeon. Finally, some clinics have a narrow specialist in joint diseases - an arthrologist.
The extent of therapeutic measures depends on the severity of the disease. If the cause of this pathology can be eliminated at an early stage, it is possible to achieve a lasting cure.
The goals of any therapy are to completely eliminate the pain, restore the destroyed cartilage, and increase the range of active movements in the joint.
The course of drug treatment is chosen only by a doctor. The patient is unable to prescribe them, as this can contribute to further destruction of the joint. The main drugs are prescribed:

- Non-steroidal anti-inflammatory tablets or ointments. Their action is aimed at relieving pain and inflammation in the affected area. Sometimes injections into the articular cavity may be prescribed.
- Products that improve blood circulation in the knee. These are muscle relaxants, antispasmodics. The latter relieves pain well.
- Products that restore articular cartilage, then improve normal nutrition.
Novocaine blockade helps relieve acute pain. The injection can be done from the outside or inside the joint. The simplest and safest way is to apply the drug externally. With proper manipulation, the pain disappears almost immediately.
An ointment based on strong NSAIDs also helps to cope with pain. Remember that you should not use strong drugs for a long time. Any medication, even the most effective, can cause side effects and allergic reactions. This means that self-medication for this serious disease is strictly not allowed.
Conservative treatment may be effective as long as the disease does not go too far. In case of irreversible damage to the joint, surgery is indicated. Metal prosthesis implantation is performed.
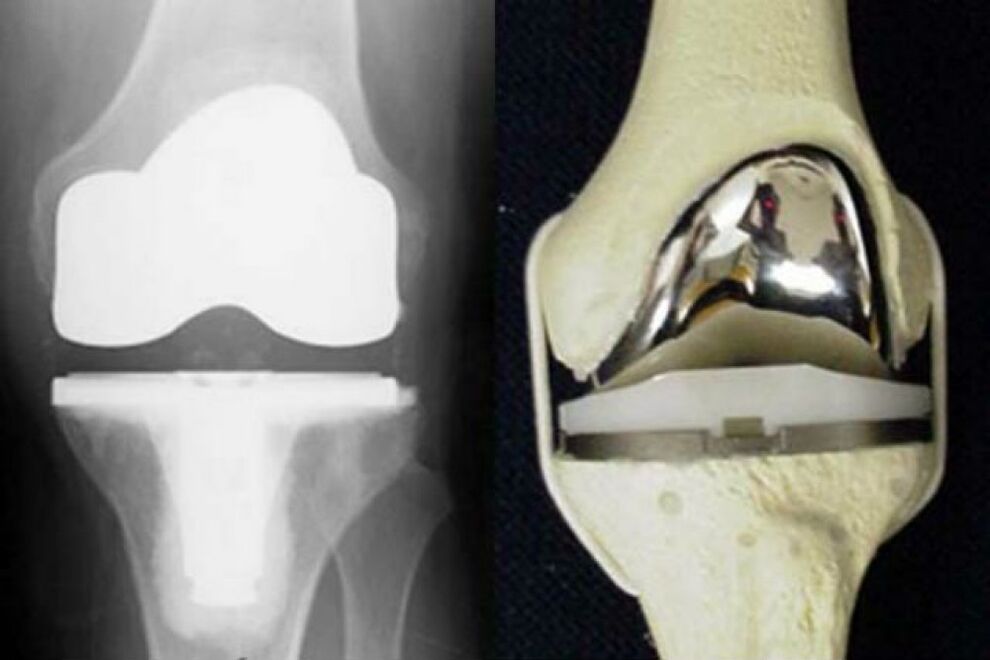
This is currently the only way to restore knee mobility. The disadvantages of these operations are the limited service life of the prosthesis and its high cost.
In arthroscopy, all surgeries are performed by microscopic punctures in the joint. Cartilage fragments, clots, etc. affected by the joint during the operation. The type of intervention described in stage 3 of the disease is ineffective.
Periarticular osteotomy is used to reduce the load. It is indicated that the joint will be done when it is not yet completely destroyed.
Reeds and orthoses are used to loosen the joint affected by the degenerative process.
The duration of treatment of the disease depends on many factors. The course of therapy with chondroprotectors can be very long - six months or more, because their effect is very slow. An experienced healthcare professional can determine how much medication you are taking.
Use of chondroprotectors in the treatment of osteoarthritis
Doctors prescribe non-steroidal anti-inflammatory drugs (NSAIDs) to relieve pain.
However, even the new generation of NSAIDs cannot prevent the spread of the pathological process. Chondroprotectors are increasingly being used to reduce the intensity of joint degeneration and restore its normal mobility.
Modern drugs in this group help to regenerate joint tissues. This is due to the presence of chondroitin in them. It is a natural component of cartilage. Regular intake of drugs of this group helps to restore it and improve health.
Despite the wide range of drugs offered, only a doctor can determine which is best for the patient. Injection of chondroprotectors is not indicated for everyone, the drugs themselves are diluted in special solvents.
If the patient follows a balanced diet and takes other medications to support the joints, dietary supplements are indicated.
The role of exercise therapy and physiotherapy in the treatment of gonarthrosis
The patient with the described pathology is strictly contraindicated in a sedentary lifestyle. For any disease of the musculoskeletal system, physical activity is simply necessary for all categories of patients. Of course, it must be dosed; Any exercise is performed only under the supervision of a physician.

A traumatologist or rehabilitation therapist individually selects specific exercises for each patient. There is no need to think that the different class kits that can be found on the internet will suit all patients without exception.
It can be really good for some, but it will do great harm for others. All loads should be gentle, aimed at the fastest and most complete restoration of the functions of the affected joints.
It is recommended to do a simple exercise at home: lift your legs while lying down, hold for a few minutes and then lower. It is harmless and can be performed even by patients with the third stage of the disease. Exercises are performed to lengthen the joint capsule under the supervision of a physician. But if it causes pain, then the execution should be stopped immediately.
Physiotherapeutic methods of treatment of the disease include:

- massage (it is strictly forbidden to do it without a doctor's prescription);
- hand therapy (should be as gentle as possible, should not cause discomfort);
- medical laser treatment;
- exposure to reflexogenic points using the finest needles;
- heat or cold treatment (still no need for heat treatment at home);
- magnetic field treatment;
- phonophoresis;
- electrophoresis;
- paraffin therapy;
- ozokerite treatment;
- moxibustion with wormwood.
Nutrition for gonarthrosis
Proper nutrition is the basis of successful treatment of degenerative diseases of the musculoskeletal system. The patient may gain weight due to a poorly designed diet. Lack of vitamins and trace elements aggravates the pathology.
All people with gonarthrosis should increase the amount of vitamins and minerals in their daily diet.
Dietitians recommend closely monitoring the caloric content of food. It is strictly forbidden to fast or follow an excessive diet. They can hurt, body weight will increase even more.
It is important to ensure a balanced breakfast. You need to eat at least five times a day. It is recommended to use fruits and bread for snacks.
The following dishes and meals are excluded:

- sweet soda;
- fatty foods;
- semi-finished products;
- spices;
- containers with taste and odor enhancers;
- fatty meat;
- fried foods;
- white cabbage;
- tomatoes and bell peppers;
- orange, lemon;
- chocolate;
- bananas, grapes (they are very high in calories).
Jellied meat and jelly are useful. They contain a lot of collagen, which helps to restore bone. Jellyed meat is prepared to contain less fat, so the amount of calories will be reduced.
For those suffering from osteoarthritis, protein sources can be dairy products - cheese, cottage cheese or kefir. It is very useful to use legumes. Be sure to include nuts in your diet.
It is necessary to follow a drinking regimen. It is recommended to consume about 2 liters of water, unless it is associated with kidney disease.
About alternative treatment of the disease
It is important to remember that traditional methods cannot replace effective methods of formal medicine. And therefore, they should be used in complex treatment, there can be no other therapy for this serious disease.
Use regular soda to eliminate swelling of the knee. The fabric is moistened with soda gruel and wrapped around the knee. Above, it is recommended to add a plastic bag to increase the heating effect. Keep the prepared compress all night.

A similar compress is made with the addition of food vinegar. Acetylsalicylic acid tablets should be taken in parallel with the application of compresses.

Burdock leaves are very useful for the knees. It is recommended to lubricate the knee with vegetable oil before applying the leaves. The leaves should have several layers.
All this is wrapped in a plastic bag. Compresses with maple leaves are prepared in the same way.
Medical bile relieves inflammation, swelling and pain. Used in the form of night warming compresses. Pay has virtually no side effects.
Treatment with honey is carried out when the patient is not allergic to it. After warming with a painful joint heating pad, lubricate with honey and give a gentle massage. After that, add the burdock leaves to the string.
Prevention of gonarthrosis
Preventing the disease is easier than treating it. Prevention measures include:
- high-quality, balanced nutrition with the use of sufficient amounts of protein, vitamins and calcium;
- elimination of bad habits;
- fight with excess weight;
- normalization of physical activity;
- prevention of joint injuries during sports or strenuous physical activity.
It is important to see a doctor immediately when the first signs of a problem appear. It is possible to find out which doctor treats gonarthrosis in a clinical consultation. It is advisable to undergo a thorough medical examination to determine the cause of the disease.
Knee osteoarthritis is a serious disease: if not taken into account, there is a risk of disability and complete immobility. To prevent this, you need to properly treat the affected joint. Early-onset therapeutic measures contribute to almost complete remission of this pathology, help maintain high performance and quality of life.



















